SBIRT is intended to be a standard of care, and as such, it should be incorporated into your standard patient procedure. The SBIRT process does not require a large time investment per patient. It is feasible to fit the various SBIRT actions into the "gaps" in your current flow in a manner that is minimally disruptive. The goal of this article is to guide you through the steps of developing an SBIRT procedure that is tailored to your clinic.
When designing a procedure, the following elements must be included:
These decisions must be made for each of the three key components of SBIRT: Prescreening, Full Screening, and Intervention. Click on the sections below to learn about each component.
You can also watch our 20 minute webinar on procedure design for further information.
Prescreening is a brief questionnaire that quickly and accurately separates your patient population into two segments: those that need SBIRT services and those that don't.
Prescreening is a time-saving mechanism. The 4-question prescreener recommended by IndianaSBIRT takes approximately 30 seconds to administer, whereas a full screening and brief intervention can take between 10 and 30 minutes. It enables you to spend your limited resources in the most effective manner.
The recommended prescreening consists of a single validated question each for alcohol and drugs, and the two-question PHQ2 for depression.
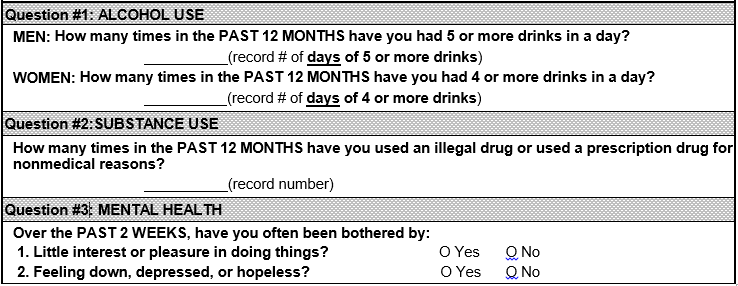
Alternatively, a 2-question prescreener containing only the alcohol and drugs questions can be used if your clinic does not plan to include depression screening in its SBIRT procedure.
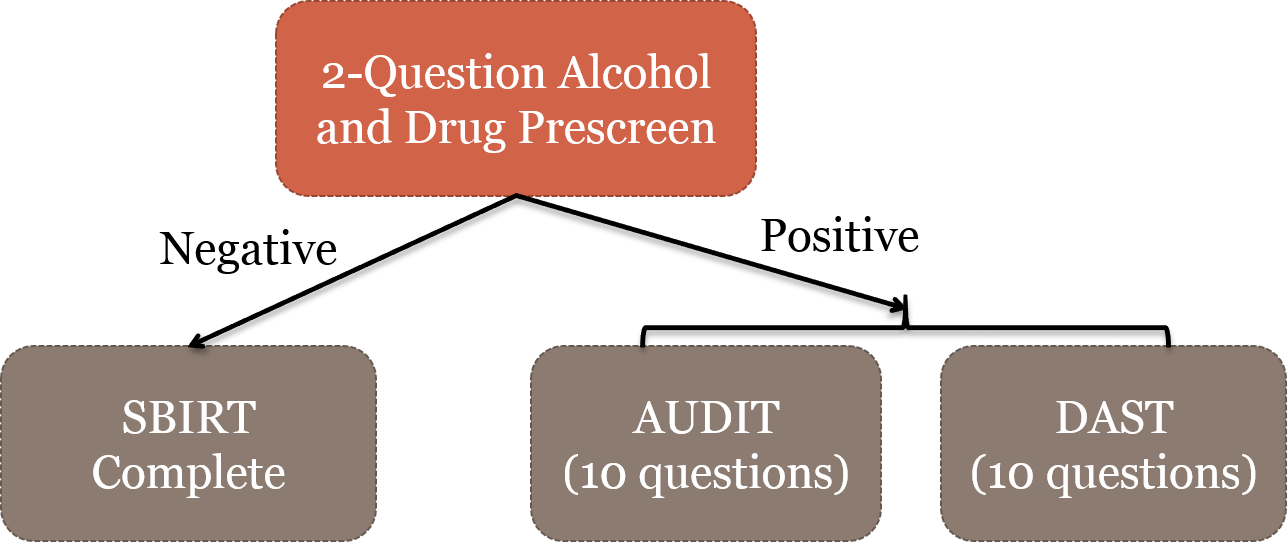
A "negative" prescreen means that the patient answered negatively to all prescreen questions and is therefore likely at minimal risk for substance-related issues. A "positive" prescreen means that at least one answer was positive.
In terms of patient flow, the SBIRT process ends for negative-scoring patients at this stage. Positive patients continue on to receive a full SBIRT screening.
IndianaSBIRT has had success using both patient self-administered prescreens and MA-administered prescreens. Both methods have advantages and disadvantages.
Patient self-administered prescreens reduces the burden of SBIRT on your MA staff. A clipboard with a paper form can be handed to the patient in the waiting room by front desk staff or a greeter. The patient completes the prescreening in the waiting room and then hands it to either the front desk or the MA when the patient is called back to do intake. Patients may also be more honest about alcohol or drug use when completing a self-administered form. When IndianaSBIRT clinics switched from MA-administered to self-administered, positive prescreen rates increased.

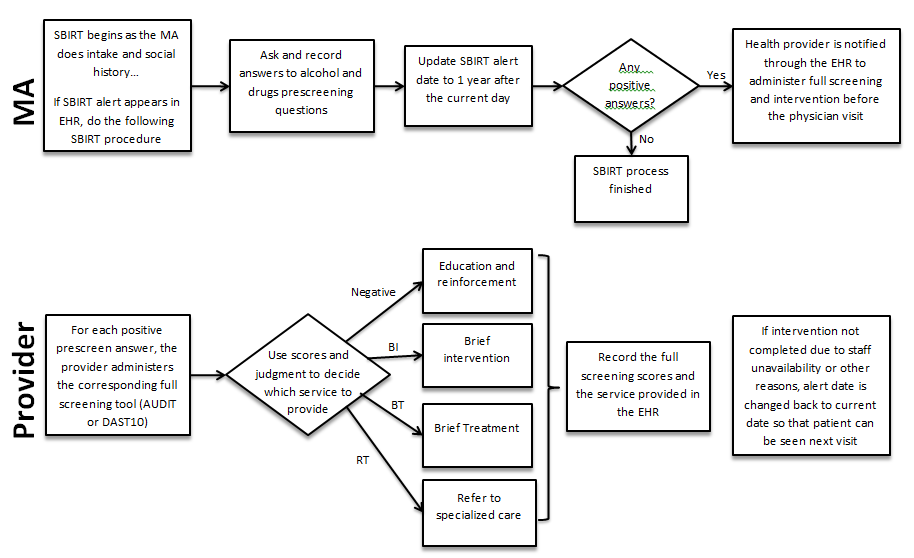
MA-administered prescreens are verbally asked by the MA after the patient has been taken to an exam or triage room. An advantage of this method is that the MA can directly enter a patient's responses into the EHR without the use of any paper forms. A disadvantage is that MAs will require additional training to ask the questions in an accurate and unbiased manner. The questions should be read word for word, because paraphrasing such as "You haven't done drugs in the past year, have you?" can bias a patient's response.
A self-administered prescreen can be given to the patient in the waiting room after front desk check-in but before an MA does intake. Or it can be given to the patient in an exam/triage room after an MA does intake but before the provider visit.
An MA-administered prescreen should be completed in an exam/triage room during intake but before the provider visit.
Prescreening (and SBIRT in general) is an annual, once-per-year process. If a patient has multiple visits within a year, SBIRT should be performed during only one of those visits. As such, a mechanism is necessary to notify staff members when they should do SBIRT and when they should not.
If your EHR supports timed alerts, they are an ideal solution. When a patient is prescreened, create an alert (or update an existing one) for one year after the current day. If the patient returns in less than a year, the alert will not appear, and SBIRT will not be performed. If the patient returns after a year, the alert will pop up, notifying the staff member to initiate the SBIRT process.
Alternatively, if your EHR does not have timed alerts but does have a date or text field in an easily accessible place in the EHR, a staff member can manually look at that date during a patient's visit to see if the patient is due for SBIRT. When prescreening is performed, that date field is updated to be one year later.

A third option is to not use dates for scheduling but instead perform SBIRT only for new patients and during annual-type visits. If your clinic performs annual wellness visits, for example, you could always conduct SBIRT during those visits and not during any other types of visits (except for new patients). This makes identifying who needs SBIRT simpler, but you will miss patients that do not attend those annual-type visits
The results of the prescreen should be recorded in the EHR. Record Yes or No for each question as the numerical score is not important. Or you can record Positive or Negative for the overall prescreen result.
A positive prescreen result must be communicated to the staff member responsible for the full screening. This communication can be done passively by recording the result in the EHR and having the next staff member check the EHR before interacting with the patient. Or it can be done actively by sending a message via the EHR, putting the paper prescreening form in a the exam room door slot, or paging the provider.
The principle behind screening is to administer one or more short screening tools that identify a patient's probabilistic level of risk and suggest what type of intervention that patient should receive. Screening is a procedure guiding mechanism.
An AUDIT score of 11, for example, indicates that a patient most likely is drinking at a risky level and should receive a brief intervention. It is always up to a provider's clinical judgment, however, to select which services to provided.
IndianaSBIRT recommends the Alcohol Use Disorders Identification Test (AUDIT) for alcohol, the 10-question Drug Abuse Screening Test (DAST-10) for drugs, and the Patient Health Questionnaire (PHQ9) for depression. If your SBIRT process does not include depression, the PHQ9 is not required.
View the instruments:
A full screening should be administered only if its associated prescreen question was positive. For example, if a patient prescreened positive for alcohol and depression, but negative for drugs, the AUDIT and PHQ9 should be administered, but the DAST10 should not be administered.
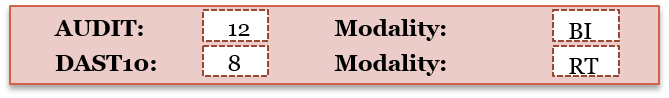
The AUDIT and the DAST-10 both have four scoring ranges or modalities that indicate a certain level of risk and a recommended service. After administering a screening, the score should be tallied to determine which modality it falls into.
AUDIT Score |
DAST-10 Score |
Modality |
0-7 |
0 |
Education and Positive Reinforcement |
8-15 |
1-2 |
Brief Intervention |
16-19 |
3-5 |
Brief Treatment |
20-40 |
6-10 |
Referral to Treatment |
If the AUDIT and DAST-10 are both administered, use the higher of the two modalities to determine the most important service to provide.
The PHQ9 does not have treatment modalities. Instead, its scoring ranges indicate the severity of depression. IndianaSBIRT generally does not use SBIRT to provide treatment for depression by itself. Depression is considered only when it is a co-occurring condition with alcohol or drug use.
The full screenings can be patient self-administered, MA-administered, or provider-administered.

IndianaSBIRT has predominantly used provider-administered full screenings. An advantage of this method is that the screenings are a chance for the provider to build rapport with the patient before beginning the intervention.
The screenings are also a chance to garner additional information about a patient's substance use. When a patient responds to the screening questions, he or she may elaborate about his or her usage habits or personal situation. If the patient or an MA completed the screening, that extra information may never reach the provider.
A downside is that the screenings take approximately 3-5 minutes to complete, and the provider may be unable to spare that extra time.
If provider-administered is not feasible, patient self-administered is the recommended second choice as it avoids the need for MA training and administration.
If the provider administers the full screening, it can be conducted in the exam room during the provider visit. If the patient or MA completes the full screening, it should be done before the provider visit.
If possible, the full screening tools should exist in the EHR. EHR integration allows a screening to be administered without the need for a paper form, and it may calculate the screening's score and modality automatically, speeding up the process.
If the screening tools cannot be programmed into the EHR in their entirety, a field to record the screening's score and/or modality should exist instead.
In terms of communication, none is required if the provider is responsible for both the full screening and the intervention. If the patient or MA completes the screening, however, the screening results must be given to the provider, most likely via the EHR or a paper form.
For positive patients, the SBIRT encounter ends with some type of intervention service. The service provided depends on a patient's level of risk, which is determined by the patient's full screening scores and the provider's clinical judgment.
The levels of service are...
To learn more about interventions and how they should be performed, take our free interactive 1-hour training modules for motivational interviewing, drug education, and SBIRT.
The intervention should be performed by a trained professional such as a physician, nurse, mental health specialist, social worker, or counsellor.

The intervention provider can be same person who is addressing the patient's primary complaint, such as the medical provider. In that case, the intervention should be done during the primary care visit.
If the intervention is performed a different staff member, such as a mental health specialist, the intervention should be done directly before or after the primary care visit. We recommend performing performing the intervention in the exam room, as sending only positive patients to a special location can be stigmatizing.
Record in the EHR the service actually performed by the provider, along with any notes.
The prescreening result, full screening modality, and service provided are all important metrics to store electronically as they can be used in statistics for project evaluation and improvement. For example, if during a month your clinic had 100 positive prescreens but only 50 full screens were administered, you know there is a breakdown in the process between the prescreening and full screening steps.
If the intervention could not be completed for any reason (lack of time or provider unavailability), flag the patient in the EHR and complete the intervention during the patient's next visit.
As an example, SBIRT has been successfully implemented in a clinic using the following procedure: